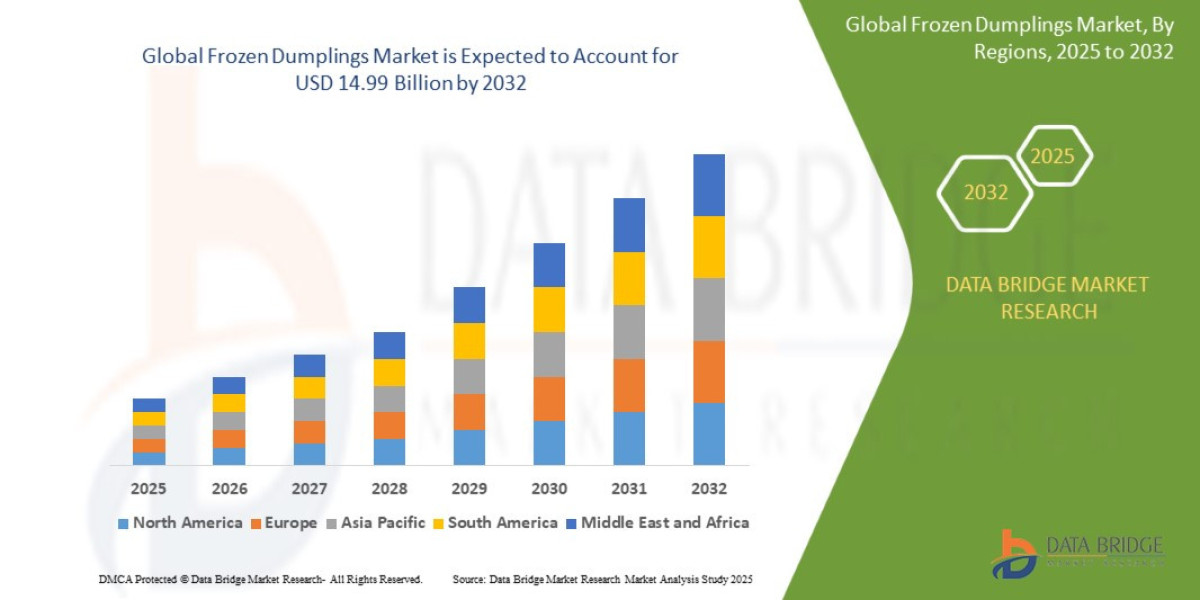
The Frozen Dumplings Market sector is undergoing rapid transformation, with significant growth and innovations expected by 2032. In-depth market research offers a thorough analysis of market size, share, and emerging trends, providing essential insights into its expansion potential. The report explores market segmentation and definitions, emphasizing key components and growth drivers. Through the use of SWOT and PESTEL analyses, it evaluates the sector’s strengths, weaknesses, opportunities, and threats, while considering political, economic, social, technological, environmental, and legal influences. Expert evaluations of competitor strategies and recent developments shed light on geographical trends and forecast the market’s future direction, creating a solid framework for strategic planning and investment decisions.
Get a Sample PDF of Report - https://www.databridgemarketresearch.com/request-a-sample/?dbmr=global-frozen-dumplings-market
Which are the top companies operating in the Frozen Dumplings Market?
The report profiles noticeable organizations working in the water purifier showcase and the triumphant methodologies received by them. It likewise reveals insights about the share held by each organization and their contribution to the market's extension. This Global Frozen Dumplings Market report provides the information of the Top Companies in Frozen Dumplings Market in the market their business strategy, financial situation etc.
CJ CheilJedang Corp. (South Korea), General Mill Inc. (U.S), Sanquan Food Co., Ltd (China), Ajinomoto Co., Inc. (Japan), Hakka (Australia), Day-Lee Foods, Inc.(U.S), Wei Chuan U.S.A., Inc. (Taiwan), Way Fong LLC (U.S), InnovAsian Cuisine Enterprises Inc. (U.S)
Report Scope and Market Segmentation
Which are the driving factors of the Frozen Dumplings Market?
The driving factors of the Frozen Dumplings Market are multifaceted and crucial for its growth and development. Technological advancements play a significant role by enhancing product efficiency, reducing costs, and introducing innovative features that cater to evolving consumer demands. Rising consumer interest and demand for keyword-related products and services further fuel market expansion. Favorable economic conditions, including increased disposable incomes, enable higher consumer spending, which benefits the market. Supportive regulatory environments, with policies that provide incentives and subsidies, also encourage growth, while globalization opens new opportunities by expanding market reach and international trade.
Frozen Dumplings Market - Competitive and Segmentation Analysis:
**Segments**
- By Type: The market for global frozen dumplings can be segmented into meat dumplings, vegetarian dumplings, and others.
- By Distribution Channel: The distribution channels for frozen dumplings include supermarkets/hypermarkets, convenience stores, online retail, and others.
- By Region: The market can be segmented into North America, Europe, Asia Pacific, Latin America, and Middle East & Africa.
**Market Players**
- Ajinomoto Co., Inc.
- Sanquan Food Co., Ltd.
- CJ Corporation
- General Mills Inc.
- Synear
- Way Fong
- Kitchen Cooked, Inc.
- Day-Lee Foods, Inc.
- CP Food Products Inc.
- Top Gourmet Food Industries
The global frozen dumplings market is expected to witness significant growth by 2029. The increasing demand for convenient and easy-to-prepare food products, alongside the rising popularity of Asian cuisine worldwide, is driving the market growth. Meat dumplings and vegetarian dumplings are the two primary segments within the market, catering to different consumer preferences. With the growing trend of healthier eating habits, there is a rising demand for vegetarian and plant-based frozen dumplings. The distribution channels for frozen dumplings play a crucial role in reaching a wider consumer base, with supermarkets/hypermarkets being the dominant channel. However, online retail is gaining traction due to the increasing preference for online shopping.
The market players in the global frozen dumplings market are key to driving innovation, quality, and variety in the product offerings. Companies like Ajinomoto Co., Inc., Sanquan Food Co., Ltd., and CJ Corporation are leading the market with their wide range of frozen dumpling products. General Mills Inc. and Synear are also prominent players in the market, known for their quality and taste consistency. Regional players such as Way Fong and Kitchen Cooked, Inc. cater to specific market segments with their unique flavors and offerings. Day-Lee Foods, Inc., CPThe global frozen dumplings market is experiencing a significant surge in demand driven by various factors, including changing consumer lifestyles, increasing preference for ready-to-eat meals, and the growing popularity of Asian cuisine across the globe. The market segmentation based on type, distribution channels, and regions provides a comprehensive view of the market landscape and opportunities for key players to capitalize on. Meat dumplings and vegetarian dumplings stand out as the primary segments within the market, with consumers showing a growing inclination towards plant-based and healthier frozen dumpling options. The diverse distribution channels, including supermarkets/hypermarkets, convenience stores, and online retail platforms, play a vital role in ensuring wide market reach and accessibility for consumers.
Among the prominent market players in the global frozen dumplings market, Ajinomoto Co., Inc., Sanquan Food Co., Ltd., and CJ Corporation emerge as leading entities driving innovation, quality, and product diversity. These players leverage their extensive product portfolios and strong market presence to cater to the evolving consumer preferences and taste profiles. General Mills Inc. and Synear also command a significant market share, known for their consistent quality standards and flavor varieties. Regional players such as Way Fong and Kitchen Cooked, Inc. bring unique flavors and offerings to specific market segments, enhancing product differentiation and catering to niche consumer preferences. Day-Lee Foods, Inc., CP Food Products Inc., and Top Gourmet Food Industries contribute to market dynamics with their distinct product offerings and market strategies, adding depth and competition to the frozen dumplings market landscape.
The market outlook for the global frozen dumplings industry points towards robust growth potential in the coming years, fueled by increasing urbanization, busy lifestyles, and the rising trend of convenience-oriented food choices. As consumer awareness regarding healthy eating habits and sustainability grows, there is a shift towards plant-based and wholesome frozen dumpling options. Market players need to focus on product innovation, packaging efficiency, and strategic partnerships to stay competitive and meet evolving consumer demands. The continued expansion of distribution channels,**Market Players**
- CJ CheilJedang Corp. (South Korea)
- General Mill Inc. (U.S)
- Sanquan Food Co., Ltd (China)
- Ajinomoto Co., Inc. (Japan)
- Hakka (Australia)
- Day-Lee Foods, Inc.(U.S)
- Wei Chuan U.S.A., Inc. (Taiwan)
- Way Fong LLC (U.S)
- InnovAsian Cuisine Enterprises Inc. (U.S)
The global frozen dumplings market is poised for significant growth in the coming years, driven by several key factors that are reshaping the industry landscape. The market segmentation based on type, distribution channels, and regions provides valuable insights into the diverse opportunities available for market players to capitalize on. Meat dumplings and vegetarian dumplings remain the dominant segments within the market, with consumers increasingly gravitating towards healthier and plant-based options. The distribution channels for frozen dumplings play a vital role in reaching a wide consumer base, with supermarkets/hypermarkets taking the lead, although online retail is gaining traction due to shifting consumer preferences.
Market players in the global frozen dumplings industry are instrumental in propelling innovation, quality, and variety in product offerings. Leading companies such as CJ CheilJedang Corp., General Mill Inc., Sanquan Food Co., Ltd, and Ajinomoto Co., Inc. are at the forefront of driving market growth with their diverse product portfolios and strong market presence. Regional players like Day-L
Explore Further Details about This Research Frozen Dumplings Market Report https://www.databridgemarketresearch.com/reports/global-frozen-dumplings-market
Key Benefits for Industry Participants and Stakeholders: –
- Industry drivers, trends, restraints, and opportunities are covered in the study.
- Neutral perspective on the Frozen Dumplings Market scenario
- Recent industry growth and new developments
- Competitive landscape and strategies of key companies
- The Historical, current, and estimated Frozen Dumplings Market size in terms of value and size
- In-depth, comprehensive analysis and forecasting of the Frozen Dumplings Market
Geographically, the detailed analysis of consumption, revenue, market share and growth rate, historical data and forecast (2024-2032) of the following regions are covered in Chapters
The countries covered in the Frozen Dumplings Market report are U.S., Canada, Mexico, Brazil, Argentina, Rest of South America, Germany, Italy, U.K., France, Spain, Netherlands, Belgium, Switzerland, Turkey, Russia, Rest of Europe, Japan, China, India, South Korea, Australia, Singapore, Malaysia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific, Saudi Arabia, U.A.E, South Africa, Egypt, Israel, and Rest of the Middle East and Africa.
Key Questions Answered:
1. What is the Frozen Dumplings Market?
2. How big is the Frozen Dumplings Market?
3. What is the growth rate of the Frozen Dumplings Market?
4. What are the key drivers of the Frozen Dumplings Market?
5. Which region dominates the Frozen Dumplings Market?
6. Who are the major players in the Frozen Dumplings Market?
7. What segments are included in the Frozen Dumplings Market?
8. What are the challenges facing the Frozen Dumplings Market?
9. What is the future outlook for the Frozen Dumplings Market?
10. How can companies benefit from the Frozen Dumplings Market?
Browse More Reports:
Asia-Pacific Dental Lasers Market – Industry Trends and Forecast
Gynecology Surgical Instruments Market – Industry Trends and Forecast
Industrial X-Ray Market – Industry Trends and Forecast
Surgical Sutures Market – Industry Trends and Forecast
North America Surgical Sutures Market – Industry Trends and Forecast
Europe Surgical Sutures Market – Industry Trends and Forecast
Asia-Pacific Surgical Sutures Market – Industry Trends and Forecast
North America Foam Insulation Market - Industry Trends and Forecast
Europe Foam Insulation Market – Industry Trends and Forecast
Asia-Pacific Foam Insulation Market – Industry Trends and Forecast
U.S. Internal Neuromodulation Devices Market - Industry Trends and Forecast
Belgium Foam Insulation Market – Industry Trends and Forecast
France Foam Insulation Market – Industry Trends and Forecast
North America Industrial X-Ray Market – Industry Trends and Forecast
Europe Industrial X-Ray Market – Industry Trends and Forecast
Data Bridge Market Research:
Today's trends are a great way to predict future events!
Data Bridge Market Research is a market research and consulting company that stands out for its innovative and distinctive approach, as well as its unmatched resilience and integrated methods. We are dedicated to identifying the best market opportunities, and providing insightful information that will help your business thrive in the marketplace. Data Bridge offers tailored solutions to complex business challenges. This facilitates a smooth decision-making process. Data Bridge was founded in Pune in 2015. It is the product of deep wisdom and experience.
Contact Us:
Data Bridge Market Research
US: +1 614 591 3140
UK: +44 845 154 9652
APAC: +653 1251 978
Email:- [email protected]