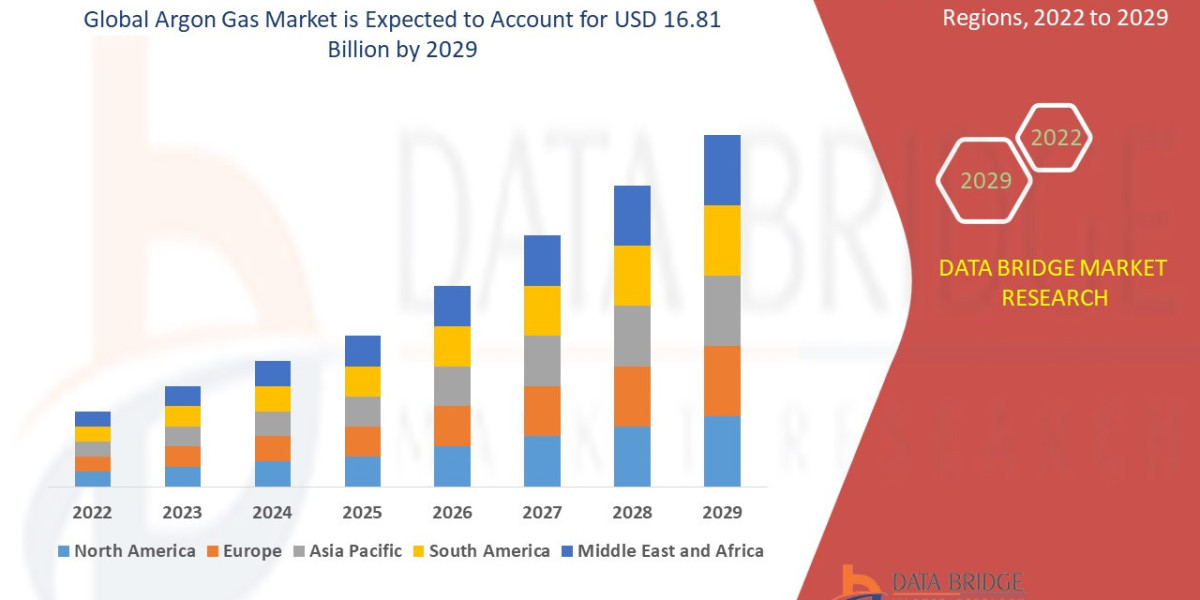
The Argon Gas Market sector is undergoing rapid transformation, with significant growth and innovations expected by 2032. In-depth market research offers a thorough analysis of market size, share, and emerging trends, providing essential insights into its expansion potential. The report explores market segmentation and definitions, emphasizing key components and growth drivers. Through the use of SWOT and PESTEL analyses, it evaluates the sector’s strengths, weaknesses, opportunities, and threats, while considering political, economic, social, technological, environmental, and legal influences. Expert evaluations of competitor strategies and recent developments shed light on geographical trends and forecast the market’s future direction, creating a solid framework for strategic planning and investment decisions.
Get a Sample PDF of Report - https://www.databridgemarketresearch.com/request-a-sample/?dbmr=global-argon-gas-market
Which are the top companies operating in the Argon Gas Market?
The report profiles noticeable organizations working in the water purifier showcase and the triumphant methodologies received by them. It likewise reveals insights about the share held by each organization and their contribution to the market's extension. This Global Argon Gas Market report provides the information of the Top Companies in Argon Gas Market in the market their business strategy, financial situation etc.
Air Products Inc., (U.S.), Linde Plc (Germany), Air Liquide (France), Ellenbarrie Industrial Gases (India), Praxair Technology, Inc., (U.S.), TAIYO NIPPON SANSO CORPORATION, (Japan), AIMS INDUSTRIES PRIVATE LIMITED (India), scicalgas (U.S.), SOL Group (Italy), Atlas Copco AB (Sweden), Zaburitz Pearl Energy Co., Ltd., (Myanmar), Rotarex (Luxembourg), Messer Group GmbH (Germany), Amico Group, (UAE) and GCE Group (Sweden)
Report Scope and Market Segmentation
Which are the driving factors of the Argon Gas Market?
The driving factors of the Argon Gas Market are multifaceted and crucial for its growth and development. Technological advancements play a significant role by enhancing product efficiency, reducing costs, and introducing innovative features that cater to evolving consumer demands. Rising consumer interest and demand for keyword-related products and services further fuel market expansion. Favorable economic conditions, including increased disposable incomes, enable higher consumer spending, which benefits the market. Supportive regulatory environments, with policies that provide incentives and subsidies, also encourage growth, while globalization opens new opportunities by expanding market reach and international trade.
Argon Gas Market - Competitive and Segmentation Analysis:
**Segments**
- By Storage, the global argon gas market can be segmented into cylinders, tonnage, and merchant liquid.
- By Function, the market can be categorized into welding, lighting, insulation, and others.
- Based on End-Use Industry, the market can be divided into metal manufacturing & fabrication, chemicals, healthcare, electronics, food & beverage, and others.
**Market Players**
- Air Liquide
- The Linde Group
- Air Products and Chemicals, Inc.
- Taiyo Nippon Sanso Corporation
- Messer Group GmbH
- Praxair Technology, Inc.
- Iwatani Corporation
- BASF SE
- Air Water, Inc.
- Ellenbarrie Industrial Gases Ltd.
The global argon gas market is expected to witness substantial growth in the forecast period of 2023-2029. The market is being primarily driven by the growing demand for argon gas in various end-use industries such as metal manufacturing & fabrication, chemicals, healthcare, electronics, and food & beverage. The welding segment is projected to dominate the market owing to the increasing use of argon gas in welding applications due to its superior inert properties. Additionally, the rising adoption of argon gas for lighting and insulation purposes is further expected to fuel market growth.
On the basis of storage, the cylinder segment is anticipated to hold a significant market share as cylinders are widely used for storing and transporting argon gas in various industries. Moreover, in terms of function, the welding segment is likely to account for a substantial share of the market due to the extensive use of argon gas in welding processes for creating an inert atmosphere to prevent oxidation.
Geographically, Asia-Pacific is expected to lead the global argon gas market during the forecast period due to the rapid industrialization and increasing construction activities in countries like China and India. The growing automotive and electronics sectors in the region are further boosting the demand for argon gas. North America and Europe are also anticipated toThe global argon gas market is poised for significant growth in the coming years, driven by several factors that are shaping the industry landscape. One key driver is the increasing demand for argon gas across a diverse range of end-use industries, including metal manufacturing & fabrication, chemicals, healthcare, electronics, and food & beverage. Argon gas is widely utilized in these sectors for various applications such as welding, lighting, and insulation, owing to its inert properties and effectiveness in creating controlled atmospheres. The welding segment, in particular, is expected to witness robust growth, fueled by the rising adoption of argon gas in welding processes to prevent oxidation and ensure high-quality welds.
In terms of storage options, cylinders are projected to dominate the market due to their widespread use in storing and transporting argon gas efficiently. The cylinder segment is expected to maintain a significant market share, driven by the convenience and portability offered by cylinders in various industrial settings. Additionally, the tonnage and merchant liquid segments are also likely to play significant roles in catering to the diverse storage needs of end-users across different industries.
From a regional perspective, Asia-Pacific is poised to emerge as a key market leader in the global argon gas market, driven by factors such as rapid industrialization, increasing construction activities, and the growing automotive and electronics sectors in countries like China and India. The region's booming industrial landscape and expanding manufacturing activities are fueling the demand for argon gas, particularly in applications such as welding and metal fabrication. North America and Europe are also expected to witness substantial growth in the argon gas market, supported by ongoing technological advancements, the presence of established market players, and a growing focus on sustainable manufacturing practices.
Key market players such as Air Liquide, The Linde Group, Air Products and Chemicals, Inc., and others are actively involved in strategic initiatives such as partnerships, collaborations, and product innovations to enhance their market presence and cater to the evolving needs of customers. These companies are focusing on expanding their product**Market Players:**
- Air Products Inc. (U.S.)
- Linde Plc (Germany)
- Air Liquide (France)
- Ellenbarrie Industrial Gases (India)
- Praxair Technology, Inc. (U.S.)
- TAIYO NIPPON SANSO CORPORATION (Japan)
- AIMS INDUSTRIES PRIVATE LIMITED (India)
- Scicalgas (U.S.)
- SOL Group (Italy)
- Atlas Copco AB (Sweden)
- Zaburitz Pearl Energy Co., Ltd. (Myanmar)
- Rotarex (Luxembourg)
- Messer Group GmbH (Germany)
- Amico Group (UAE)
- GCE Group (Sweden)
The global argon gas market is positioned for significant growth in the forecast period of 2023-2029, driven by the escalating demand for argon gas in key end-use industries such as metal manufacturing & fabrication, chemicals, healthcare, electronics, and food & beverage. The welding segment is expected to maintain its dominance in the market, propelled by the increasing utilization of argon gas for welding applications due to its inert properties. Moreover, the adoption of argon gas for lighting and insulation purposes is set to further stimulate market expansion.
In terms of storage options, cylinders are projected to hold a significant market share due to their widespread use in storing and transporting argon gas efficiently. The welding segment, on the other hand, is expected to account for a substantial share of the market
Explore Further Details about This Research Argon Gas Market Report https://www.databridgemarketresearch.com/reports/global-argon-gas-market
Key Benefits for Industry Participants and Stakeholders: –
- Industry drivers, trends, restraints, and opportunities are covered in the study.
- Neutral perspective on the Argon Gas Market scenario
- Recent industry growth and new developments
- Competitive landscape and strategies of key companies
- The Historical, current, and estimated Argon Gas Market size in terms of value and size
- In-depth, comprehensive analysis and forecasting of the Argon Gas Market
Geographically, the detailed analysis of consumption, revenue, market share and growth rate, historical data and forecast (2024-2032) of the following regions are covered in Chapters
The countries covered in the Argon Gas Market report are U.S., Canada, Mexico, Brazil, Argentina, Rest of South America, Germany, Italy, U.K., France, Spain, Netherlands, Belgium, Switzerland, Turkey, Russia, Rest of Europe, Japan, China, India, South Korea, Australia, Singapore, Malaysia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific, Saudi Arabia, U.A.E, South Africa, Egypt, Israel, and Rest of the Middle East and Africa.
Key Questions Answered:
1. What is the Argon Gas Market?
2. How big is the Argon Gas Market?
3. What is the growth rate of the Argon Gas Market?
4. What are the key drivers of the Argon Gas Market?
5. Which region dominates the Argon Gas Market?
6. Who are the major players in the Argon Gas Market?
7. What segments are included in the Argon Gas Market?
8. What are the challenges facing the Argon Gas Market?
9. What is the future outlook for the Argon Gas Market?
10. How can companies benefit from the Argon Gas Market?
Browse More Reports:
Middle East and Africa Automotive Logistics Market – Industry Trends and Forecast
North America Automotive Logistics Market – Industry Trends and Forecast
Pharmaceutical Contract Packaging Market – Industry Trends and Forecast
Data Center Security Market – Industry Trends and Forecast
Data Center Storage Market – Industry Trends and Forecast
Power Distribution Unit (PDU) Market – Industry Trends and Forecast
Laser Ablation Systems Market – Industry Trends and Forecast
Base Metal Mining Market – Industry Trends and Forecast
Titanium Market – Industry Trends and Forecast
Medical Specialty Bags Market – Industry Trends and Forecast
Medicated Confectionery Market – Industry Trends and Forecast
Petri Dish Fillers Market – Industry Trends and Forecast
Butanediol Market – Industry Trends and Forecast
Laser Safety Goggles Market – Industry Trends and Forecast
Sauces Market – Industry Trends and Forecast
Substitute Natural Gas Market – Industry Trends and Forecast
Data Bridge Market Research:
Today's trends are a great way to predict future events!
Data Bridge Market Research is a market research and consulting company that stands out for its innovative and distinctive approach, as well as its unmatched resilience and integrated methods. We are dedicated to identifying the best market opportunities, and providing insightful information that will help your business thrive in the marketplace. Data Bridge offers tailored solutions to complex business challenges. This facilitates a smooth decision-making process. Data Bridge was founded in Pune in 2015. It is the product of deep wisdom and experience.
Contact Us:
Data Bridge Market Research
US: +1 614 591 3140
UK: +44 845 154 9652
APAC: +653 1251 978
Email:- [email protected]