Failed Back Syndrome (FBS), also known as Failed Back Surgery Syndrome (FBSS), is a complex condition that often leaves patients experiencing chronic pain even after spinal surgery. This persistent discomfort can not only affect physical health but also significantly impact emotional well-being, mental health, and overall quality of life. In this blog, we will explore the causes, symptoms, and treatment options for FBS, along with the broader implications it has on patients’ lives.
What is Failed Back Syndrome?
Failed Back Syndrome is not a single specific condition but rather a collection of symptoms that arise after spinal surgery, where the expected improvements, such as pain relief or better mobility, are not achieved. FBS doesn't necessarily mean the surgery itself failed, but that the anticipated outcomes were not realized.
Common symptoms of FBS include:
Persistent or recurring back pain
Sciatica (radiating leg pain)
Muscle spasms
Limited range of motion
Emotional distress, such as anxiety or depression
How Common is FBS?
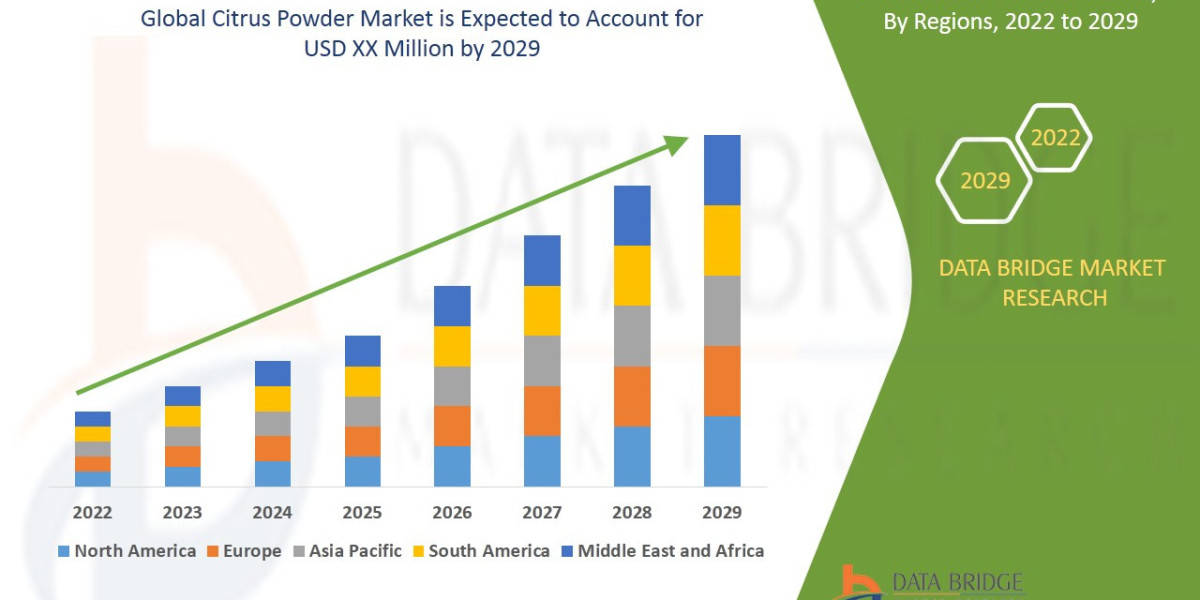
Research indicates that Failed Back Syndrome affects approximately 10-40% of patients who undergo spinal surgeries, with the prevalence varying based on the type of procedure and underlying conditions. Despite advancements in surgical methods, FBS remains a significant challenge in spinal care.
Causes and Risk Factors of FBS
Understanding the underlying causes and risk factors of FBS is crucial for both prevention and management. These factors can be divided into surgical and patient-related categories.
Surgical Factors
Incorrect Diagnosis: Misidentifying the root cause of back pain can lead to ineffective surgical procedures.
Incomplete Procedure: Inadequate decompression or incomplete removal of herniated discs can leave symptoms unresolved.
Scar Tissue Formation: Epidural fibrosis, or scar tissue near nerve roots, can cause persistent pain.
Hardware Problems: Issues with surgical implants, such as improper placement or failure, may lead to complications.
Patient-Related Factors
Pre-existing Conditions: Conditions like diabetes, obesity, and osteoporosis can interfere with healing and recovery.
Psychological Factors: Anxiety, depression, and pain-related fear can worsen symptoms and hinder healing.
Lifestyle Choices: Smoking, poor nutrition, and lack of physical activity can contribute to unfavorable surgical outcomes.
The Impact of FBS on Quality of Life
Failed Back Syndrome can affect nearly every aspect of a patient’s life, creating a ripple effect on physical, emotional, and social well-being.
Physical Limitations
Chronic pain can severely limit mobility, making even simple tasks like walking, bending, or lifting difficult. Over time, this can lead to muscle weakness, weight gain, and a decreased ability to carry out daily activities.
Emotional and Mental Health
Living with persistent pain can lead to emotional struggles. Studies show that people with FBS often experience:
Depression: Feelings of being trapped in a cycle of pain and failed treatments can be emotionally devastating.
Anxiety: Worries about further surgery or worsening symptoms contribute to elevated anxiety.
Sleep Disruptions: Chronic pain often causes difficulty sleeping, leading to fatigue, irritability, and a reduced quality of life.
Social and Financial Strain
FBS can make it difficult to engage in work, hobbies, or social activities, leading to isolation. Additionally, the financial burden of ongoing medical treatments, therapies, and medications can put a strain on relationships and personal finances.
Managing Failed Back Syndrome: Innovative Treatment Options
While treating FBS can be challenging, there are various medical interventions and strategies that offer hope for better outcomes and improved quality of life.
Non-Surgical Approaches
Physical Therapy: Customized exercise programs designed to strengthen muscles and enhance flexibility. Techniques like water therapy and yoga are also effective for chronic pain management.
Pain Management: Medications such as NSAIDs, muscle relaxants, and antidepressants can help alleviate pain. Injections like nerve blocks and epidural steroid shots offer targeted relief.
Psychological Support: Cognitive Behavioral Therapy (CBT) can help patients manage negative thought patterns. Support groups provide emotional and social connections to others facing similar challenges.
Minimally Invasive Procedures
Spinal Cord Stimulation (SCS): This technique involves implanting an electrical device near the spinal cord to block pain signals. Studies show that SCS can significantly reduce pain and improve mobility.
Radiofrequency Ablation (RFA): This procedure uses heat to disrupt nerve signals, providing effective pain relief for localized pain.
Advanced Surgical Options
If conservative treatments fail, more invasive surgeries may be considered, such as:
Spinal Fusion Revision: Revisiting issues with prior fusion surgeries to correct underlying problems.
Dynamic Stabilization: Flexible implants are used to stabilize the spine while preserving natural motion.
Conclusion
Failed Back Syndrome is a life-altering condition that affects millions of people worldwide. Though its impact on physical, emotional, and social well-being is profound, a combination of medical interventions, lifestyle changes, and emotional support can help patients manage symptoms and improve quality of life. Ongoing research and emerging treatments continue to offer hope for those dealing with FBS. Remember, every patient’s journey is unique, and with the right care and support, significant improvements in well-being are possible.